Gut-Brain Balance Calculator
Your Gut-Brain Score
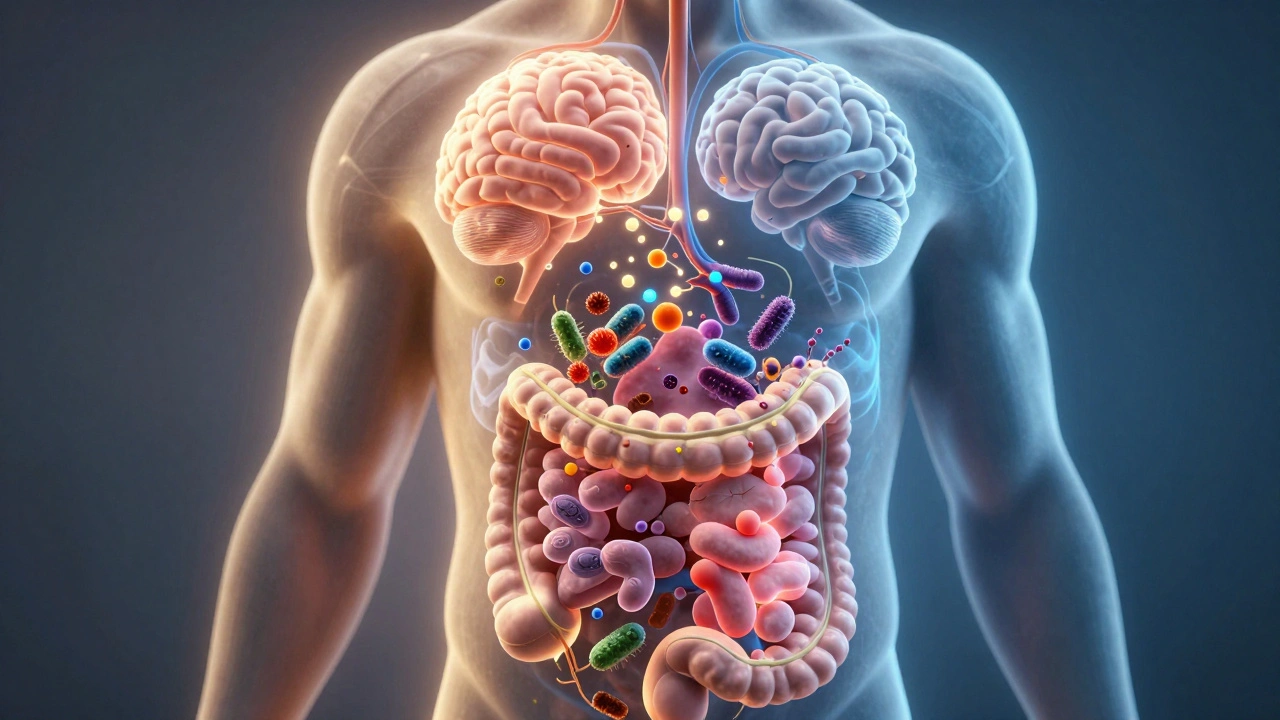
When you feel anxious before a big meeting, do you also get a knot in your stomach? That’s not just in your head-it’s your gut talking. The connection between your digestive system and your mood isn’t coincidence. It’s biology. Over the last decade, scientists have uncovered a powerful two-way street between your gut and your brain, and what happens in your intestines can directly shape how you feel emotionally.
Your gut has its own nervous system
Most people think of the brain as the boss of your body. But your gut has its own complex network of neurons-over 100 million of them-called the enteric nervous system. It’s often called the "second brain" because it can operate independently, controlling digestion, blood flow, and enzyme release without input from your skull. This system doesn’t just digest food. It sends signals straight to your brain through the vagus nerve, the main highway connecting gut and brain.
Studies from the University of California, Los Angeles and the University of Cork in Ireland show that people with irritable bowel syndrome (IBS) are three times more likely to have anxiety or depression than those with healthy digestion. The reverse is also true: people with chronic stress or depression often develop stomach pain, bloating, or constipation-even when no physical cause is found.
The microbiome: your gut’s invisible residents
Your gut is home to trillions of bacteria, viruses, and fungi-collectively called the microbiome. These tiny organisms aren’t just along for the ride. They produce chemicals that influence your mood. One of the most important is serotonin. About 90% of your body’s serotonin, the neurotransmitter linked to happiness and calm, is made in your gut. Not your brain. Your gut.
These microbes also make gamma-aminobutyric acid (GABA), which reduces anxiety, and short-chain fatty acids like butyrate, which reduce inflammation in the brain. When your microbiome is out of balance-called dysbiosis-these signals get scrambled. A 2023 study in Nature Microbiology found that people with major depressive disorder had significantly lower levels of two key gut bacteria: Faecalibacterium prausnitzii and Bifidobacterium.
Antibiotics, processed foods, chronic stress, and lack of sleep can all wipe out these helpful bugs. Once they’re gone, it’s not easy to bring them back. That’s why gut health isn’t just about avoiding stomach upset-it’s about protecting your mental resilience.
Food isn’t just fuel-it’s a message
What you eat doesn’t just feed your body. It feeds your gut bacteria. And what they eat determines what they send to your brain.
Diets high in sugar, fried foods, and refined carbs feed harmful bacteria that trigger inflammation. That inflammation doesn’t stay in your gut. It travels through your bloodstream and crosses into your brain, where it can interfere with neurotransmitter production and even shrink areas linked to memory and emotional control.
On the flip side, fiber-rich foods-like oats, lentils, broccoli, apples, and bananas-feed the good bacteria. Fermented foods like kimchi, sauerkraut, kefir, and plain yogurt introduce live cultures that can help restore balance. A 2024 clinical trial in Melbourne found that participants who ate 10 servings of fiber-rich foods and 2 servings of fermented foods daily for eight weeks reported a 32% drop in anxiety symptoms and improved sleep quality.
You don’t need a perfect diet. But if you’re constantly eating white bread, sugary snacks, and takeout, your gut-and your mood-are paying the price.

Stress doesn’t just hurt your mind-it hurts your gut
When you’re stressed, your body releases cortisol and adrenaline. These hormones slow digestion, reduce blood flow to the gut, and change the way your microbiome behaves. In short: stress turns your gut into a war zone.
Chronic stress is linked to leaky gut syndrome, where the lining of your intestines becomes more permeable. This lets toxins and undigested food particles escape into your bloodstream, triggering immune responses that lead to brain inflammation. That’s one reason why people under long-term stress often develop food sensitivities, bloating, or sudden IBS flare-ups.
And here’s the catch: the more your gut is inflamed, the more your brain feels under attack. It’s a loop. Stress → gut damage → inflammation → brain changes → more anxiety → more gut damage.
Breaking this loop isn’t about meditating your way to a perfect gut. It’s about addressing both sides at once. Movement, deep breathing, and sleep aren’t just "mental health" practices-they’re gut repair tools.
What actually helps? Evidence-backed steps
Trying to fix your gut for better mental health doesn’t mean buying expensive supplements or following fad diets. Real change comes from simple, consistent habits:
- Eat more fiber. Aim for 30 grams a day. That’s 1 cup of lentils, 2 apples, 1 cup of oats, and a handful of almonds.
- Include fermented foods daily. Even 2 tablespoons of sauerkraut or a small cup of kefir helps.
- Reduce ultra-processed foods. If it comes in a bag with a long list of unpronounceable ingredients, it’s likely feeding bad bacteria.
- Move your body. Just 20 minutes of walking a day improves gut motility and reduces stress hormones.
- Get enough sleep. Poor sleep changes your microbiome within 48 hours. Aim for 7-8 hours.
These aren’t quick fixes. But after six weeks of doing even three of these, most people notice less bloating, fewer mood swings, and more mental clarity.
When to see a professional
If you’ve tried dietary changes and still struggle with both gut symptoms and anxiety or low mood, it’s time to talk to a doctor or registered dietitian. Some conditions-like small intestinal bacterial overgrowth (SIBO), celiac disease, or chronic gastritis-can mimic mental health issues but need medical treatment.
Specialists now use stool tests to analyze microbiome balance and blood markers to check for inflammation. In some cases, targeted probiotics or low-FODMAP diets under supervision make a big difference. Don’t assume it’s "all in your head." Your gut is sending real signals.
The bigger picture
For years, mental health was treated as separate from physical health. But science is clear: your brain doesn’t live in isolation. It’s deeply connected to your gut. The way you eat, sleep, move, and manage stress doesn’t just affect your digestion-it shapes your anxiety, your focus, and your emotional resilience.
This isn’t about blaming yourself for feeling down. It’s about recognizing that healing your gut can be part of healing your mind. And that’s powerful. You don’t need a pill to change your mood. Sometimes, you just need better food, more sleep, and a little patience.
Start small. One extra serving of veggies. One less sugary snack. One extra hour of sleep. Your gut-and your brain-will thank you.
Can gut health really cause depression?
Yes, research shows a strong link. People with imbalanced gut bacteria often have lower levels of mood-regulating chemicals like serotonin and GABA. Inflammation from gut issues can also spread to the brain, affecting areas tied to emotion and motivation. While gut health alone doesn’t cause depression, it can significantly contribute to its development and severity.
Do probiotic supplements help with anxiety?
Some strains do-especially Lactobacillus and Bifidobacterium species. But not all probiotics are the same. A 2023 meta-analysis in JAMA Psychiatry found that specific probiotic blends reduced anxiety symptoms in clinical trials, but only when taken consistently for at least 4 weeks. Supplements aren’t magic pills-they work best when paired with dietary fiber and lifestyle changes.
How long does it take to improve gut health for mental benefits?
You can start noticing changes in as little as two weeks-like less bloating or better sleep. But meaningful improvements in mood and anxiety usually take 6 to 8 weeks of consistent habits. The gut microbiome is slow to shift, but once it does, the benefits last.
Can stress alone damage your gut?
Absolutely. Chronic stress reduces stomach acid, slows digestion, and weakens the gut lining. It also changes which bacteria thrive in your gut, favoring inflammatory strains. Even without poor diet, long-term stress can lead to leaky gut, IBS symptoms, and food intolerances.
Is there a test to check my gut-brain connection?
There’s no single test, but doctors can check for gut inflammation (via blood tests like CRP), microbiome balance (through stool tests), and food sensitivities. Some clinics now offer gut-brain axis assessments that combine symptom tracking, dietary logs, and lab markers to build a full picture. If you’re struggling with both gut and mental symptoms, ask for a referral to a gastroenterologist or integrative health specialist.