Alcohol Impact on Gut Health Calculator
Enter your alcohol consumption details and click "Analyze Gut Impact" to see how it affects your gut health.
Gut Health Effects Overview
Ever wonder why a night out sometimes leaves you feeling bloated, gassy, or just plain off? The culprit is often more than just a hangover-it’s the way alcohol gut health interactions can throw your digestive system off balance. Below we break down what happens in the gut when you drink, why it matters for long‑term wellbeing, and what you can do to keep things running smoothly.
What Alcohol Does Inside Your Gut
When you sip a drink, about 20% of the alcohol is absorbed directly through the stomach lining; the rest makes its way to the small intestine where most absorption occurs. Alcohol is a volatile compound that diffuses quickly across cell membranes, disrupting normal cellular function. This rapid entry means the gut is the first line of exposure, and the gut’s own community of microbes feels the impact almost immediately.
Alcohol Meets the Gut Microbiome
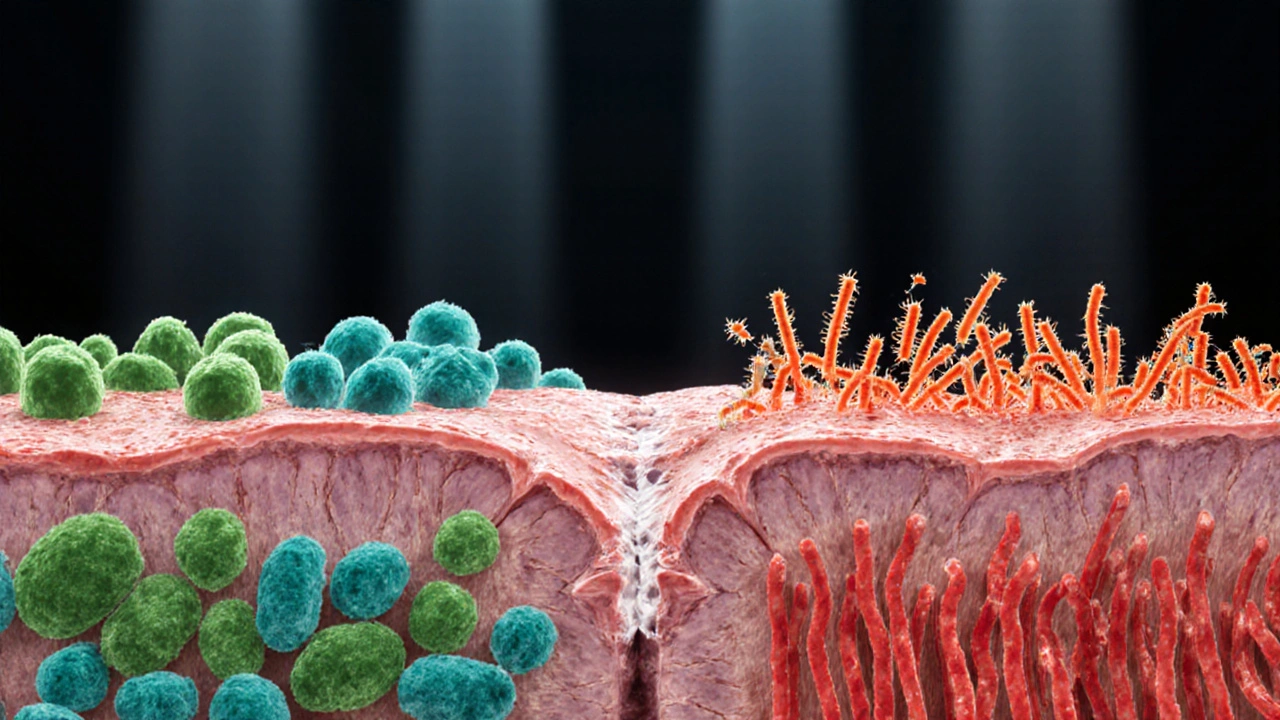
Gut microbiome is a complex ecosystem of bacteria, fungi, and viruses that live in the gastrointestinal tract and help digest food, synthesize vitamins, and regulate immunity. Studies from 2023‑2024 show that even moderate drinking can reduce beneficial bacteria like Lactobacillus and Bifidobacterium> by up to 30%, while encouraging growth of opportunistic species such as Enterobacteriaceae. These shifts weaken the microbiome’s ability to produce short‑chain fatty acids (SCFAs), especially butyrate, a key fuel for colon cells.
Damaging the Intestinal Lining
The gut wall consists of a single layer of epithelial cells sealed together by tight junction proteins. Intestinal lining is a protective barrier that regulates nutrient absorption and keeps harmful substances out. Alcohol metabolites, particularly acetaldehyde, interfere with these tight junctions, making them leaky. When the barrier becomes porous, larger particles-including bacterial toxins-can slip into the bloodstream, a condition commonly called "leaky gut syndrome."
Immediate Digestive Upset
- Increased gastric acid production leads to heartburn or gastritis.
- Delayed gastric emptying can cause nausea and a feeling of fullness.
- Reduced secretion of digestive enzymes such as amylase and lipase hampers breakdown of carbs and fats.
These effects are why you often experience a "butterfly" feeling in your stomach after a few drinks. The disruption also impairs absorption of nutrients like vitamin B12, magnesium, and zinc, setting the stage for deficiency symptoms.
Long‑Term Risks: From Inflammation to Disease
Regular heavy drinking amplifies the short‑term issues into chronic conditions:
- Inflammatory bowel disease is a group of disorders, including Crohn's disease and ulcerative colitis, characterized by persistent inflammation of the gastrointestinal tract. Alcohol‑induced dysbiosis and barrier breakdown increase the risk of flare‑ups.
- Leaky gut raises systemic inflammation, contributing to insulin resistance, fatty liver disease, and even mood disorders.
- The gut‑liver axis-where gut‑derived toxins travel to the liver via the portal vein-means a compromised gut can accelerate alcoholic liver disease.
Mitigating the Damage
If you enjoy a glass of wine or a weekend beer, you don’t have to quit altogether. Here are evidence‑backed steps to protect your gut while still having fun:
- Stay hydrated. Water dilutes alcohol concentration and supports mucosal protection.
- Eat fiber‑rich foods before drinking. Whole grains, legumes, and veggies provide pre‑biotics that feed beneficial microbes.
- Include probiotic‑rich foods. Yogurt, kefir, sauerkraut, and kimchi replenish probiotics are live microorganisms that confer health benefits when consumed in adequate amounts. A daily dose of 10‑20billion CFU can counteract dysbiosis.
- Consider digestive enzyme supplements. Enzymes labeled for "alcohol metabolism" often contain bromelain or papain, which help break down proteins and reduce gastric irritation.
- Limit binge patterns. Keeping blood alcohol concentration below 0.05% (roughly two standard drinks for most adults) minimizes acetaldehyde buildup.
Quick Checklist: Gut‑Friendly Drinking
| Aspect | Short‑Term (≤ 24hrs) | Long‑Term (≥ 6months) |
|---|---|---|
| Microbial Balance | Reduced Lactobacillus, ↑Enterobacteriaceae | Persistent dysbiosis, lower SCFA production |
| Intestinal Barrier | Transient loosened tight junctions | Chronic leaky gut, systemic inflammation |
| Digestive Enzymes | Decreased amylase & lipase activity | Reduced nutrient absorption, deficiencies |
| Health Outcomes | Heartburn, nausea, bloating | IBD flare‑ups, fatty liver, metabolic syndrome |
When to Seek Professional Help
If you notice any of the following, it’s time to talk to a doctor or gastroenterologist:
- Persistent abdominal pain lasting more than two weeks.
- Unexplained weight loss or chronic diarrhea.
- Frequent heartburn despite over‑the‑counter antacids.
- Blood in stool or black, tarry stools.
Early diagnosis can prevent irreversible gut damage and guide personalized treatment-often a mix of dietary changes, targeted probiotics, and, if needed, medication.
Frequently Asked Questions
Can occasional wine really harm my gut?
A single glass of wine (≈150ml) is unlikely to cause lasting damage if you’re otherwise healthy. The risk rises when alcohol is consumed on an empty stomach or in larger quantities, which can temporarily disrupt the microbiome and increase gut permeability.
Do all types of alcohol affect the gut the same way?
The core culprit is ethanol, which behaves similarly across spirits, beer, and wine. However, higher‑proof drinks deliver more ethanol per volume, leading to faster acetaldehyde buildup. Some flavored liqueurs also contain additives that can further irritate the lining.
How long does it take for the gut to recover after a binge?
Recovery varies. In most healthy adults, the microbiome begins to rebalance within 48‑72hours if you resume a fiber‑rich diet and stay hydrated. Tight‑junction proteins may need up to a week to fully restore, especially after repeated binge episodes.
Are probiotic supplements effective for alcohol‑related gut issues?
Yes, when chosen wisely. Strains like Lactobacillus rhamnosus GG and Bifidobacterium longum have been shown to reduce alcohol‑induced inflammation and improve barrier integrity. Look for products delivering at least 10billion CFU per dose and containing multiple strains.
What diet supports gut healing after heavy drinking?
Focus on anti‑inflammatory foods: plenty of leafy greens, fermented veggies, lean protein, and omega‑3 rich fish. Limit processed sugars and fried foods, which can exacerbate dysbiosis. A daily 25‑30g fiber intake is a good target for rebuilding microbial diversity.

